Tooth decay (dental caries) is a prevalent dental disorder marked by the destruction of tooth structure due to the acidic by-products produced by bacteria metabolising sugars in the mouth. The process leads to demineralisation and degradation of the hard tissues of the teeth, such as enamel and dentin. Tooth decay symptoms, treatment, and causes must be identified and known to prevent progressing to severe complications, such as pain, infection, and tooth loss.
The symptoms of tooth decay depend on the location and severity of the decay. The most prominent indicators are toothache, sensitivity to sweet, hot, or cold foods and beverages, visible holes or pits in the teeth, and staining on the surfaces of the teeth. Additional symptoms include persistent lousy odour, an unpleasant taste in the mouth, bleeding gums, facial swelling, and pain when biting, mainly if the decay results in an infection.
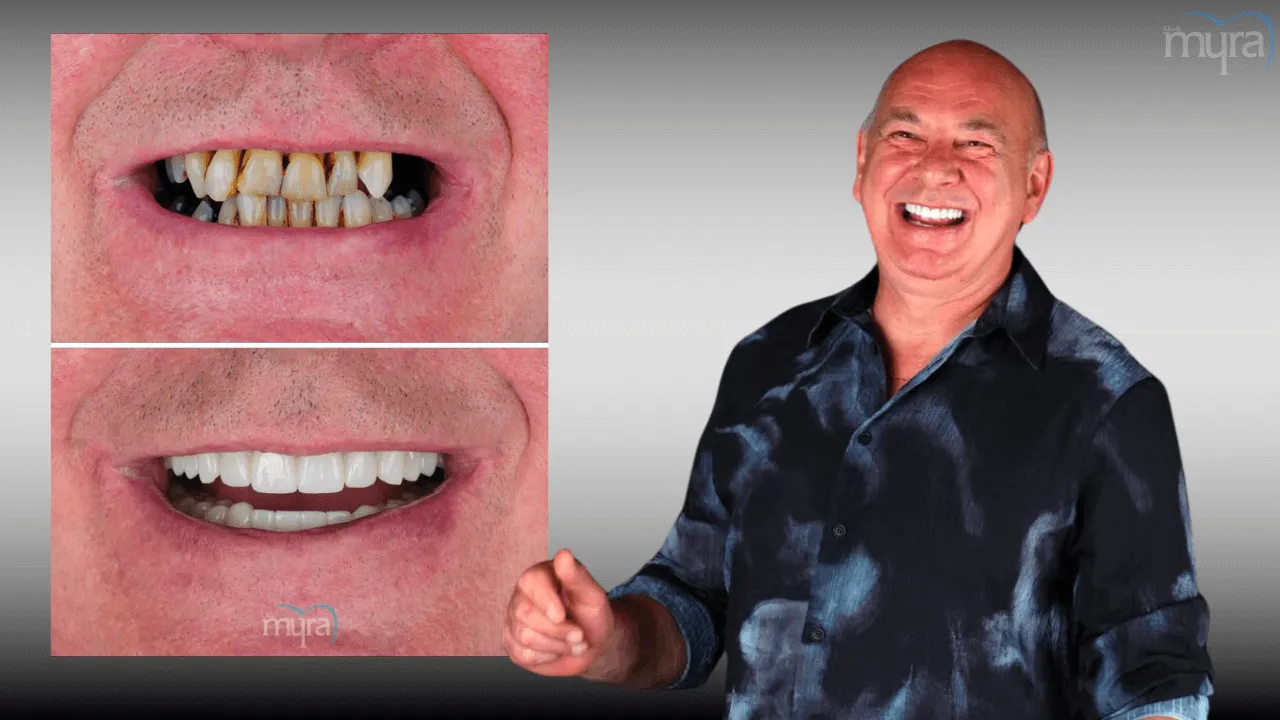
The treatment of tooth decay depends on its severity and progression. Fluoride treatments remineralise the enamel during the early phases. Interventions such as dental fillings, crowns, or root canals are necessary for more advanced decay. These procedures remove the decayed material and restore the tooth with synthetic materials. Tooth extractions are required, followed by dental implants or bridge placement to fill the gaps and restore function in severe instances.
Bacterial activity is the primary cause of tooth decay, as it converts dietary carbohydrates into acids. The bacterial activity initiates the formation of dental plaque, an adhesive biofilm that adheres to the teeth. Plaque acids have the potential to degrade tooth enamel, resulting in decay, if they are not eliminated. Certain medical conditions that affect saliva production or composition, frequent nibbling on sugary or starchy foods, dry mouth conditions, and poor oral hygiene increase the risk.
The study "Impact of Candida albicans on Oral Microbial Dysbiosis and Root Caries" by Du, et al. demonstrated that the cariogenicity of Candida albicans is reduced, and microbial balance is restored by deleting the PHR2 gene. The "Plant-mediated Synthesis of Silver-doped Zinc Oxide Nanoparticles" research of Mortezagholi, et al. has shown that nanoparticles possess improved antibacterial properties against Streptococcus mutans, implying their potential application in dental care in the future. The "Prevention of Early Childhood Caries (ECC)" study by Peng and McGrath discovered that the risk of caries in children is substantially reduced by fluoridated water and dietary supplements, and the incidence is reduced by caregiver oral health education. A deep learning model that accurately identifies and classifies dental caries with high precision was developed in Lakshmi and Chitra's "Tooth Decay Prediction and Classification from X-Ray Images using Deep CNN" research.

What are the Types of Tooth Decay?
The types of tooth decay are listed below.
- Smooth Surface Decay: Smooth surface decay emerges on the flat, smooth textures of the teeth, predominantly on the sides adjacent to the teeth. The decay initiates when plaque accumulates on smooth surfaces, producing acids that progressively demineralise the enamel.
- Pit and Fissure Decay: Pit and fissure decay forms in the grooves and crevices on the occlusal surfaces of the posterior teeth, molars, and premolars. It happens because food residue and bacteria entrap in hard-to-clean areas produce acid, which in turn causes enamel degradation.
- Root Decay: Root decay forms on the root surfaces of teeth, mainly in individuals with receding gums. Exposure of the tooth roots to plaque and acids, with their absence of protective enamel, leads to rapid demineralisation and cavity formation.
- Coronal Decay: Coronal decay occurs on the occlusal surfaces or between the teeth, affecting the tooth's crown, the visible part. It is the most prevalent type of decay and results from the interaction of plaque bacteria with sugars, making acids that erode the enamel and dentin.
- Recurrent Decay: Recurrent decay occurs around existing fillings, crowns, or other dental restorations. It is induced by plaque bacteria infiltrating the margins of restorations, leading to further demineralisation and decay of the surrounding tooth structure.
- Incipient Decay: Incipient decay is the initial stage of tooth decay, characterised by white spots on the enamel. It involves preliminary demineralisation caused by acid from plaque bacteria but has not yet advanced to form cavities and is usually changed with appropriate oral brushing, flossing, and fluoride therapy.

What are the Symptoms of Tooth Decay?
The symptoms of tooth decay are listed below.
- Toothache: A toothache is a persistent or intermittent pain in or around a tooth. It occurs due to dental pulp inflammation, instigated by a bacterial infection or advanced caries, which irritates the nerves.
- Tooth Sensitivity: Tooth sensitivity is discomfort or pain in response to thermal or sweet stimuli. It is precipitated by the exposure of dentin, the substrate beneath the enamel, owing to erosion or cavities, allowing external stimuli to penetrate the sensitive inner layers of the tooth.
- Pain When Eating/Drinking: Pain when eating or drinking is mild to acute when ingesting sweet, hot, or cold foods and beverages. It ensues because the protective enamel is compromised, permitting irritants to intrude upon the sensitive dentin and pulp, resulting in discomfort.
- Visible Holes: Visible holes are cavities or observable pits in the teeth. These are caused by destroying enamel and dentin from bacterial acid production, creating noticeable cavities on the tooth surface.
- Staining: Staining is the presence of brown, black, or white discolourations on any surface of a tooth. The staining occurs due to the accumulation of plaque and tartar or the breakdown of the tooth structure from decay, altering the tooth’s appearance.
- Pain When Biting: Pain when biting is discomfort experienced when applying pressure on a tooth. It is caused by decay reaching the pulp or by a cracked tooth, creating pressure on the inflamed or damaged area, resulting in sharp pain.
- Bad Breath: Bad breath is an unpleasant odour emanating from the mouth. It is induced by bacterial buildup and food particles trapped in cavities or between teeth, producing foul-smelling compounds.
- Bad Taste: Bad taste is a persistent unpleasant taste in the mouth. It is a consequence of decaying food debris and bacterial byproducts producing a metallic or sour taste.
- Bleeding Gums: Bleeding gums bleed easily, especially during brushing or flossing. They occur due to inflammation from plaque buildup at the gum line, leading to gingivitis or periodontal disease, which makes the gums more susceptible to bleeding.
- Facial Swelling: Facial swelling is the swelling around the face or jaw. It happens when an infection from a decayed tooth spreads to the surrounding tissues, causing inflammation and fluid accumulation.

What are the Causes Tooth Decay?
The causes of tooth decay are listed below.
- Bacterial Activity: Bacteria produce acids by metabolising carbohydrates and starches in the oral cavity. The metabolic process initiates dental decay, as the acids directly attack the enamel of the teeth.
- Dietary Carbohydrates: Oral microorganisms utilise sugary and starchy foods, such as cereals, breads, candies, and fruits, as substrates. Bacteria facilitate the production of harmful acids by breaking down these carbohydrates when ingested.
- Dental Plaque: Dental plaque is a biofilm that develops on the teeth due to a combination of bacteria, dietary particles, acids, and saliva. The plaque hardens and permits acids to persistently contact tooth enamel, resulting in caries if it is not removed through proper oral hygiene.
- Acid Erosion: The acids produced by bacterial metabolism within the plaque gradually erode tooth enamel, progressively weakening it, leading to cavities.
- Inadequate Oral Hygiene: Plaque and confined food particles are not removed from the teeth and gum line by insufficient brushing and flossing. The risk of decay is elevated by the sustained action of acids on the enamel, which is facilitated by poor oral hygiene practices.
- Regular Consumption of Snacks: Regular snack consumption, particularly sugary or starchy snacks, provides a continuous food source for bacteria, resulting in more frequent acid assaults on tooth enamel. Frequent exposure to acid expedites tooth decay.
- Dry Mouth: Saliva neutralises acids produced by bacteria in the mouth and dietary particles. Inadequate saliva production elevates tooth erosion, precipitated by conditions such as xerostomia or specific medications.
- Medical Conditions: The risk of dental decay is elevated by certain diseases, such as diabetes, due to elevated glucose levels in the saliva, which provides food for oral bacteria. Gastroesophageal reflux disease (GERD) causes stomach acids to ascend to the oral cavity, where they cause tooth injury.

What are the Treatments of Tooth Decay?
The treatments of tooth decay are listed below.
- Fluoride Treatments: Fluoride remedies are effective in the early phases of tooth decay when the cavity is just beginning to form. The treatments potentially change earlier deterioration by enhancing the remineralisation of tooth enamel. Professional therapies, available in liquids, gels, foams, or varnishes, contain a higher concentration of fluoride than over-the-counter fluoride sources, accelerating the fortification of enamel.
- Dental Fillings: Dental fillings or restorations are the primary treatment for cavities that have progressed beyond the earliest stage. Composite resin, porcelain, or dental amalgam, a combination of several metals, are fillings to replace decayed tooth material. The treatment prevents further decay by sealing off spaces where bacteria penetrate, restoring the integrity and function of the tooth.
- Dental Crowns: Crowns are advised for teeth that have been significantly decayed or compromised. A crown is a custom-made covering that replaces the entire visible portion of the tooth, reinforcing its structure and reducing the likelihood of fracture. Crowns are manufactured from materials such as gold, high-strength porcelain, resin, or porcelain fused to metal.
- Root Canals: A root canal is required when erosion infiltrates the pulp, which is the innermost portion of the tooth that contains blood vessels and nerves. The infected pulp is removed, the root canal is cleaned to eradicate the infection, and the tooth's structure and function are restored by filling the canal. A root canal treatment prevents teeth from being extracted by addressing the underlying infection and decay.
- Tooth Extractions: Extraction is the only option when decay has caused irreversible damage to a tooth. Removing a tooth results in alignment issues with the remaining teeth due to the displacement. Options such as dental implants or bridges are considered to bridge the breach and reestablish dental function following an extraction.
- Sealants: Dental sealants are another preventive treatment frequently employed to safeguard teeth from decay. Sealants are applied to the chewing surfaces of the back teeth molars to prevent food and bacteria from lodging in the grooves and fissures of the enamel, substantially reducing the risk of cavities in the treated areas.
Can Tooth Decay Be Treated At Home?
No, tooth decay cannot be treated at home. Home remedies, such as improved oral hygiene practices such as brushing with fluoride toothpaste and flossing, help remove plaque and reduce bacterial load. These approaches are inadequate to repair the damage or rebuild the tooth structure once decay has taken hold.
Professional dental remedies are indispensable for treating tooth decay. For example, a dentist administers fluoride treatments during the initial phases of decay to assist in remineralising the enamel and prevent further decay. Only a dental professional administers fluoride varnish or gel, which is significantly more concentrated than over-the-counter products.
Therapeutic procedures, such as fillings, are necessary for more advanced degeneration. Dentists extract the decayed portion of the tooth and fill the cavity with materials such as gold, amalgam, or composite resin. These materials prevent further decay and potential tooth loss, which restore the tooth's function and integrity.
A root canal treatment is required when erosion has penetrated the tooth's interior, resulting in an infection. The procedure entails the removal of the infected dentin, disinfection of the root canals, and sealing the canals to prevent the spread of disease. The skills and apparatus of a dental professional are necessary to perform such intricate work, which is done outside of home.
Serious complications, such as infection dissemination to other body regions, severe pain, and abscesses, result from untreated tooth decay. These concerns underscore the significance of obtaining professional care promptly.

What are the Researches about Tooth Decay?
The research about tooth decay explores the microbial causes, preventative strategies, antimicrobial treatments, and advanced diagnostic techniques of tooth decay.
Impact of Candida albicans on Oral Microbial Dysbiosis and Root Caries investigated the prevalence of Candida albicans in dental plaque from individuals with root carious lesions and without dental caries to examine its impact on root caries development. The research demonstrated that the acidogenicity of the biofilm was substantially increased in diseased sites, which exacerbated tooth demineralisation and promoted the colonisation of Candida albicans. In vitro and animal investigations have shown that the PHR2 gene is essential for the cariogenicity-promoting activity of Candida albicans. Deleting the gene resulted in a microbial equilibrium and a decrease in biofilm cariogenicity, emphasising the critical function of the fungal species in the progression of root caries.
Researchers employed an environmentally favourable method to synthesise silver-doped zinc oxide nanoparticles in Plant-mediated Synthesis of Silver-doped Zinc Oxide Nanoparticles research. The researchers evaluated their antimicrobial efficacy against Streptococcus mutans, a critical bacterium in tooth decay. The inclusion of silver allowed the nanoparticles to show better antibacterial capabilities than zinc oxide. It implies that silver-doped zinc oxide nanoparticles are a potent new antibacterial agent for preventing dental caries, mainly against the bacteria that cause tooth cavities.
The study Prevention of Early Childhood Caries (ECC) was conducted to examine the risk and protective factors for dental caries in children under six. The review synthesised findings from observational studies and randomized controlled trials and incorporated data from numerous databases, including PubMed and Medline. It was determined that fluoridated water and dietary supplements substantially reduce the prevalence of early childhood caries. Providing oral health education to caregivers effectively reduced the incidence of early childhood caries in children, underscoring the significance of preventive measures in managing early childhood dental health.
A dental disease prediction model was recently developed in a study entitled Tooth Decay Prediction and Classification from X-Ray Images using Deep CNN that utilized deep convolutional neural networks (CNNs) to process dental X-ray images. The model implemented sophisticated image segmentation methodologies to improve the precision of dental caries diagnosis. The research demonstrates that deep learning techniques effectively identify and classify dental caries from X-ray images, providing a significant tool for the early detection and management of dental diseases, with a prediction accuracy of 98%.
What are the Differences between Tooth Decay and Bad Breath?
The differences between tooth decay and bad breath are found in their causes and treatments. Tooth decay (cavities) occurs when acids produced by bacteria in the mouth damage tooth enamel. Acid production is accelerated by poor dental hygiene, frequent snacking, and sugary drinks. Tooth decay symptoms include noticeable pits or holes in the teeth, toothaches, and sensitivity to hot, cold, or sweet meals. Dentists treat dental decay by filling cavities, crowning badly damaged teeth, performing root canals if decay has reached the pulp, and extracting teeth that are not healed.
Bad breath (halitosis) is caused by poor oral hygiene, which permits food particles, plaque, and bacteria to collect in the mouth. Other factors include dry mouth, eating foods such as onions and garlic, smoking, and having gum disease or sinus infections. The primary sign of bad breath is a persistent, unpleasant odour from the mouth. Dentists advise maintaining proper dental hygiene by brushing, flossing, and using mouthwash regularly to treat bad breath. Dentists treat underlying health issues, promote hydration, and advise against foods and activities contributing to foul breath.
Tooth decay and poor breath are detrimental to oral health and underscore the necessity of basic dental care. The conditions are unpleasant and uncomfortable if not properly handled. Regular dental check-ups, thorough brushing and flossing, and a nutritious diet are critical for avoiding these problems. Early identification and personalised treatment strategies assist in effectively managing tooth decay and bad breath, guaranteeing optimal oral health.







