An endodontist is a dental professional focusing on detecting and treating pulp and root abnormalities within teeth. They have a dental degree and specialise in endodontics, particularly root canal therapy, apicoectomy, and retreatment of previously treated teeth. An endodontist is sometimes called a “root canal dentist.” Endodontists use cutting-edge treatments to address pain and suffering caused by pulp and root disorders. They are educated to handle complicated cases such as molars with many canals, anatomic abnormalities, and teeth undergoing endodontic procedures.
Endodontists treat complex cases of dental trauma, such as broken or chipped teeth, and undertake endodontic surgeries, such as apicoectomies, to address problems that are not treatable with traditional root canal procedures. They are excellent in diagnosing and treating oral pain, frequently using modern imaging techniques to pinpoint the source of discomfort. Their specialised expertise allows them to save natural teeth that otherwise need to be extracted, which improves patients' long-term oral health.
Endodontists are competent in using microscopes to achieve accurate treatment and better results. They are dental specialists who identify and treat complex reasons for tooth pain. Make an appointment with an endodontist when experiencing persistent discomfort in the teeth or mouth. They help determine what is causing the condition and undertake medical procedures to alleviate pain or discomfort. The procedures provide symptom relief while preserving the natural tooth.

What is an Endodontist?
An endodontist is a dental specialist who detects and treats pulp and root issues. Endodontists are experts in complex tooth disorders that affect the pulp. Tooth “pulp” refers to the nerves, blood vessels, and other tissues found deep within each tooth. The portion of the teeth that is visible when looking at the mirror is called enamel. An endodontist or a “root canal specialist” employs modern procedures to treat tooth pulp and root problems. The root is the component of a tooth that extends below the gums and keeps it in place. They work to relieve tooth or mouth discomfort while preserving the natural tooth at times.
Endodontists are a type of dental specialist who perform root canal therapy, apicoectomy, and dental retreatment. Endodontists are one of the types of dental specialists educated to use microscopes for accurate treatment and improved outcomes. They detect and treat dental injuries, utilise contemporary methods, control pain, and perform endodontic surgery. They treat various pulp and root issues, including infected pulp, abscesses, and traumas. Endodontists must have excellent manual dexterity and precise hand movements.
A licenced endodontist must get a dentistry degree from an approved university involving academic and clinical training. Basic knowledge aids in diagnosing and treating patients needing complex endodontic treatment. It includes managing traumatised and immature teeth, performing surgical procedures on the tooth root and surrounding tissues, and performing complex root canal treatments, including failed treatment. Gain hands-on experience in endodontics through residency programmes, education courses, and mentorships that help them develop their clinical abilities, judgement, and decision-making. Endodontists have various skills, including technical dentistry, medical knowledge, and transferable soft skills.
Ongoing education allows endodontists to keep updated on technology, materials, and techniques, improving clinical skills, patient outcomes, and professional competency. It contributes to the retention of competitiveness and expanding employment opportunities in the dental industry. The training lets prosthodontists discuss complicated dental problems while applying modern techniques and materials to get the best patient outcomes.
What is Endodontics?
Endodontics studies the basic and clinical sciences of the normal dental pulp, including the aetiology, diagnosis, prevention, and treatment of dental pulp illnesses and injuries and associated “periradicular” disorders. It derives from the Greek roots “endo” (inside) and “odont” (tooth). Endodontics is keeping a portion or the entire tooth pulp in good health or removing the entire pulp in the event of irreparable illness. It comprises teeth with irreversibly inflamed or diseased pulpal tissue. Endodontics involves not solely treating teeth with a dental pulp but rehabilitating teeth with non-surgical endodontic treatments or teeth that have developed new lesions, such as when root canal re-treatment is required or periradicular surgery. Endodontic treatment is among the most prevalent procedures. Endodontic treatment is necessary to save a tooth if the dental pulp (which contains nerves, arterioles, venules, lymphatic tissue, and fibrous tissue) becomes sick or injured.
Pulpitis is one of the most common problems caused by extensive decay, repetitive dental operations, or tooth damage. Pulpitis causes significant pain and sensitivity, necessitating root canal therapy to remove the inflamed pulp and save the tooth. Dental abscesses, or pus pockets caused by bacterial infections within the pulp chamber, are another prevalent endodontic condition. Abscesses produce severe pain, oedema, and systemic signs such as fever. Endodontic therapy, such as draining the abscess and conducting a root canal, is essential to remove the infection and keep it from spreading.
Endodontics addresses cracked or shattered teeth. Cracks expose the pulp to microorganisms, causing infection and needing treatment to save the tooth and relieve discomfort. Endodontists deal with difficulties resulting from unsuccessful previous root canal operations, where persistent infection or incorrect healing necessitates retreatment to ensure the tooth's health. Catastrophic dental injuries are common endodontic issues, including dislodged or avulsed (knocked-out) teeth. The injuries necessitate immediate and specialised care to reimplant and stabilise the tooth, ensuring the best possible chance of recovery and long-term retention.
What does an Endodontist do?
An endodontist identifies and treats problems with the dental pulp and the tissues surrounding a tooth's roots. Their job is to administer root canal therapy, a surgery to save teeth damaged by infection or injury. Endodontists are experts at diagnosing and treating complicated dental diseases. They use meticulous procedures to preserve natural teeth and avoid needing extractions. The endodontist is the one who does root canals by removing the infected or inflamed pulp, cleaning and disinfecting the inside of the tooth, and then filling and sealing it to prevent further infection. The method reduces discomfort while preserving the native tooth, which is always preferable to extraction. Endodontists treat many difficult dental conditions besides root canals. They treat catastrophic dental injuries, such as cracked, shattered, or knocked-out teeth, using specialised procedures to repair and stabilise them.
Endodontists conduct endodontic retreatment, redoing a previous root canal that did not heal well or acquired new complications. They are proficient in surgical techniques such as apicoectomy, which involves removing and sealing the tip of the tooth's root to prevent recurrent infection. Digital imaging, operating microscopes, and ultrasonic devices are just a few examples of the cutting-edge technology and methods endodontists use to provide accurate and effective treatment. Their vast knowledge and experience managing complicated dental diseases guarantee that patients receive the best treatment for issues affecting their teeth's inner structures. Their specialised care relieves pain, contributes to dental health and safeguards healthy teeth for a long time.
What is the Importance of Endodontists?
The importance of endodontists is critical in managing complex dental diseases. They provide specialised care that promotes both immediate and long-term oral health. Patients benefit from their expertise whenever feasible, which improves their general health and quality of life. Endodontists are essential in dental healthcare because they specialise in diagnosing and treating disorders with the tooth pulp and root tissues, the most complex and painful dental conditions. Their knowledge is crucial for protecting natural teeth from severe decay, infections, or damage that results in tooth loss. Endodontists salvage damaged but viable teeth through procedures such as root canal therapy, preserving the patient's natural bite and oral health.
Endodontists are essential for more than just pain alleviation. They help prevent the spread of infections, which lead to more severe health problems if not managed. Dental infections sometimes cause systemic illnesses that affect other regions of the body. Prevention is critical for overall wellness. Endodontists preserve the mouth's structure and function, which is necessary for proper chewing, speaking, and maintaining facial aesthetics. Endodontists help ensure the long-term success of dental procedures. Their specialised knowledge of the latest technology and techniques ensures that procedures are completed with high precision, lowering the risk of problems and the need for additional treatments. Their skills improve patient oral health and increase the longevity of dental work, resulting in better long-term oral health and fewer dental visits over time.
Is there a Difference between Endodontists and General Dentists?
Yes, there is a difference between endodontists and general dentists. An endodontist is a professional who performs root canals. Endodontists specialise in treating tooth pain, whereas dentists polish teeth, fix cavities, and place sealants. There are differences in their extent of practice, training, and areas of specialisation. General dentists offer comprehensive dental care treatments, such as cleanings, exams, fillings, crowns, and tooth extractions. They prioritise preserving general oral health, preventing dental disorders, and resolving common dental ailments. Most patients' primary dental care providers are general dentists, handling most of their regular dental requirements.
Endodontists are dental professionals who specialise in identifying and treating problems with tooth pulp and root tissues. Their specialised training allows them to conduct sophisticated procedures, such as root canal therapy, endodontic retreatment, and endodontic surgery, outside conventional dentistry's competence. Endodontists use cutting-edge methods and technologies, including operating microscopes and digital imaging, to provide accurate and successful treatment for tooth discomfort, infection, and injury.
General dentists conduct some basic endodontic operations, such as root canals, but they usually refer more complex cases to endodontists. It guarantees that patients receive the best care possible for complex and challenging dental conditions by using endodontists' specialised abilities and experience. Endodontists are adept at caring for the most challenging diseases affecting the inner structures of teeth, although ordinary dentists are essential for maintaining oral health.
What are the Reasons for seeing an Endodontist?
The reasons for seeing an endodontist are listed below.
- Inflammation in Teeth or Gums: The inflammation indicates an infected or inflamed tooth pulp, necessitating the specialised care endodontists give through operations such as root canal therapy to eliminate the infection and prevent subsequent issues.
- Unexplained Discomfort in Jaw or Mouth: Inexplicable pain in the jaw or mouth is another reason to see an endodontist. The discomfort indicates underlying disorders, such as abscesses or trauma to the tooth roots, requiring an endodontist's diagnostic and therapeutic expertise.
- Persistent Toothache: An urgent and common reason to see an endodontist is a persistent toothache. A toothache indicates a more severe issue, such as nerve damage or pulp infection, if it does not go away with routine dental care. Endodontists are excellent at recognising the underlying reasons for persistent pain and delivering focused therapy to reduce it.
- Teeth Sensitivity to Hot, Cold, and Sweet Meals: Endodontic treatment is necessary when teeth are sensitive to hot, cold, and sweet foods. The discomfort shows that the tooth pulp is weakened due to decay, fissures, or other conditions that endodontists are equipped to address. Their specialised treatments help lessen or eliminate sensitivity, restoring comfort and functionality to damaged teeth.
- Dental Trauma: Suffering from dental trauma is another reason to see an endodontist. Specialised care is necessary to repair and stabilise teeth broken or fractured in an accident. Endodontists are prepared to manage such emergencies and use advanced methods to save and replace damaged teeth.
- Failed Dental Treatment: A visit to an endodontist is recommended if earlier dental procedures have failed. For example, a root canal or other dental procedure that has not healed correctly or resulted in new issues is addressed and appropriately healed with endodontic retreatment, which an endodontist performs. Their experience managing complex cases ensures patients receive the best treatment for reoccurring problems

What to Expect at the Endodontist?
A comprehensive and specialised dental experience focused on detecting and treating problems with the dental pulp and root tissues is to be expected when seeing an endodontist. The session starts with a lengthy discussion of the symptoms and dental history, followed by a thorough examination. An endodontist utilises innovative diagnostic devices like digital radiography or three-dimensional imaging to provide an unobstructed image of the affected area.
The endodontist assures comfort during the process, whether a root canal, endodontic retreatment, or treatment for a tooth injury, and numbs the affected area with local anaesthesia. They use equipment and techniques to treat the problem with precision. A root canal procedure includes removing the infected or inflamed pulp, washing and sanitising the inside of the tooth, and filling and sealing it to prevent further infection.
The majority of endodontic treatments are performed on an outpatient basis. Patients have minimal discomfort following a root canal procedure. Some feel healthy enough to go back to work the same day. The mouth or tooth remains sore for many days following the surgery. More extensive surgery results in more severe or prolonged discomfort. The doctor prescribes medication to alleviate the pain, fight infection, or aid healing.
The endodontist ensures patients understand the treatment and what to expect by reviewing each procedure step with them and answering their questions. Patients receive extensive aftercare instructions to support healing and preserve dental health after the operation. Follow-up visits must be scheduled to assess the development and ensure the treatment's effectiveness.
What is the Average Cost of an Endodontist Treatment?
The average cost of an endodontic treatment is less than £50. The treatment costs vary depending on the complexity of the procedure, the tooth being treated, and the dental office's location. Diagnostic exams, X-rays, and follow-up appointments can add a few hundred dollars to the total cost. An endodontic retreatment is more expensive due to the increased complexity and time necessary to repair previous procedures. Dental insurance sometimes helps with some of such expenses, but coverage varies, and patients end up responsible for a portion of them. Endodontic treatment is an essential investment in oral health, often avoiding the need for more comprehensive and costly operations such as replacement with implants or bridges.
A single root canal tooth costs £35.99, which includes an X-ray and a lifetime guarantee as a bonus. Patients anticipate completing their course of treatment in just one clinic visit, making it an appealing option for people seeking high-quality dental care. The cost increases to £60 per canal, and one to three clinic consultations are required if more than one root canal needs to be treated. Patients continue to enjoy the affordability and high quality of care Myra Dental Clinic gives, although the cost reflects the additional complexity and time required. The clinic aims to provide comprehensive, custom-designed root canal therapy focusing on long-term dental health and patient satisfaction.
Who is not a Suitable Candidate for Endodontic Treatment?
Patients with poor oral health care and some existing illnesses are not suitable candidates for endodontic treatment. Endodontic therapy is not appropriate for everyone, and some criteria determine it. Patients with impaired immune systems or serious underlying health issues that complicate surgery or recovery are suitable candidates. Individuals with uncontrolled diabetes, recent heart surgery, or other severe medical conditions encounter more dangers during and after the procedure.
An endodontic procedure is not recommended if a tooth is too severely decaying or damaged to be repaired. Instances where the infection has spread too far to guarantee adequate treatment or if the tooth structure is too fragile to support the restoration fall under such criteria. Patients with a history of poor oral hygiene and unwillingness to maintain good dental care post-treatment are unsuitable, as the effectiveness of endodontic procedures relies on the patient's continued oral hygiene habits. Endodontic treatment does not deliver the intended results for patients who do not adhere to the required post-procedure care and checkups. Alternative therapies, including extractions or other dental surgeries, are considered.
How do Endodontists Diagnose a Tooth?
Endodontists diagnose a tooth by following the “endodontic diagnostic tests” listed below.
- Begin with a visual examination that has to be performed by the endodontist or a “root canal doctor” to check for symptoms such as an uneven bite, asymmetric facial features, or indications of infection. It is not the primary source of diagnostic information, but there are some obvious indications that a “trained eye” like an endodontist detects fast. They discuss symptoms, where and when there is discomfort, and other elements related to entire health and history.
- Identify the main complaint and check the medical history. The most crucial initial step in making a diagnosis is for the endodontist to grasp the history of the symptoms. The endodontist speaks with patients and asks questions, so patients must answer honestly.
- Get the “imaging,” which is crucial in dentistry, especially endodontics. Modern techniques, including digital radiography and cone beam 3D technology, allow patients to see what is happening inside teeth.
- Examine the sinus track. The endodontist evaluates the sinuses by performing a sinogram, which is an X-ray examination of the sinuses. The X-ray is obtained after the endodontist puts a substance known as “gutta percha” into the sinus hole. It allows the dentist to examine the state of the sinus system, which is the source of tooth pain.
- Do the vital pulp testing, in which endodontists utilise temperature, electric, and cavity testing to determine the health of a patient's tooth pulp. The pulp contains sensitive nerves that are sometimes healthy, irritated, or diseased. Endodontists disinfect the pulp during root canals and perform cervical thermal testing. Feedback on the response's degree, length, and urgency is critical to effective treatment.
- Administer periapical tests. The endodontist conducts “periapical tests” to evaluate the patient's bite. Some exams use percussion or palpation. The percussion test is the first testing approach that provides clinical evidence of “apical periodontitis.” Palpation assesses tenderness, swelling, fluctuation, hardness, and crepitation in the underlying tissues. Finding an infected tooth determines the extent of the illness. Patients struggle to describe the source of their discomfort because of “proprioceptors” in the pulp. The periodontal ligament contains proprioceptors, which make it easier to identify pain sites using percussion and palpation testing. Endodontists employ mild equipment to perform examinations to deliver good care and treatment.
What are the Procedures done by Endodontists?
The procedures done by endodontists are listed below.
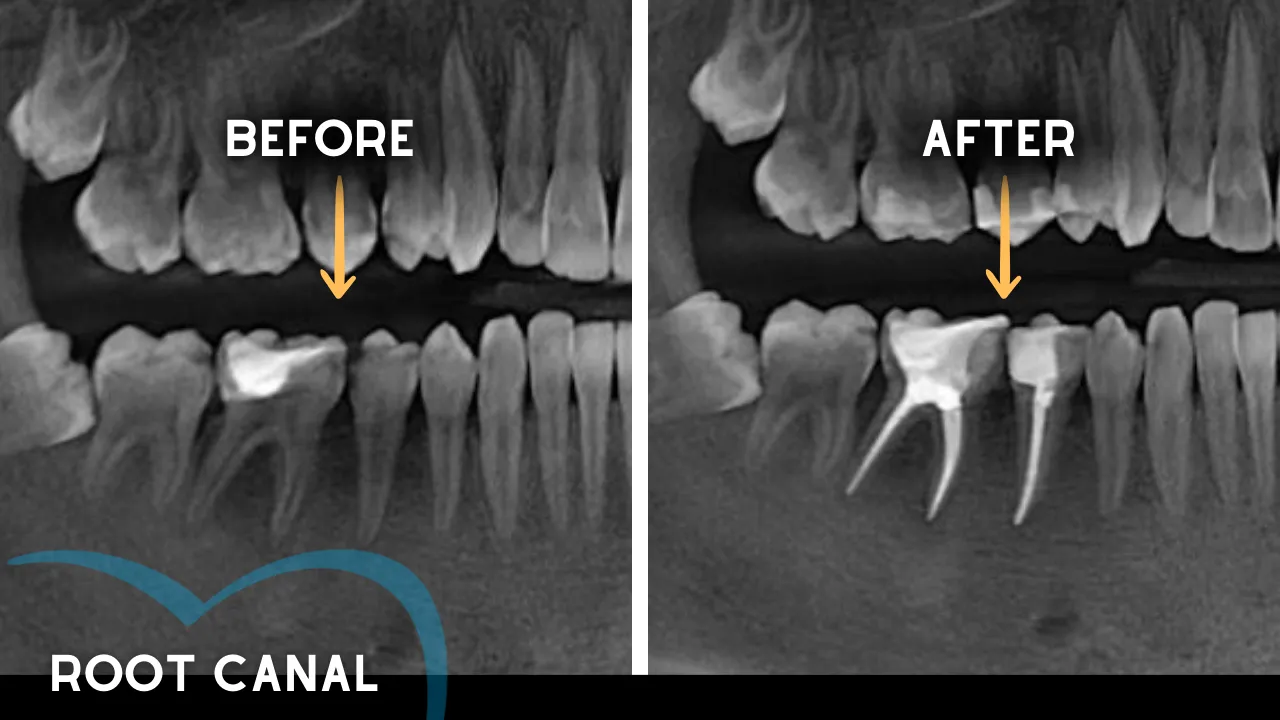
- Root Canal: A root canal is a frequent treatment in which the endodontist extracts the infected or inflammatory pulp from within the tooth. The root canals are cleaned, disinfected, and shaped before being filled and sealed with biocompatible material. This therapy relieves discomfort while saving the native tooth from extraction.
- Endodontic Retreatment: Endodontic retreatment occurs when a tooth that has received canal treatment does not recover correctly or experiences additional problems. The procedure involves reopening the tooth, removing the old filling material, cleaning and reshaping the canals, and refilling and sealing them to resolve the issue.
- Endodontic Surgery: Endodontic surgery, known as apicoectomy, is the surgical removal of the tip of the tooth's root (apex) and the surrounding diseased tissue. The method is utilised when traditional root canal therapy is insufficient to clear the infection or inflammation.
- Emergency Dental Surgery: Endodontists perform emergency dental procedures to treat acute tooth pain, infections, or traumatic injuries. Operations involve emptying abscesses, mending fractures, or anchoring dislodged teeth to provide instant relief and prevent subsequent issues.
- Tooth Extraction: Endodontists work to preserve teeth, but in cases where a tooth is too damaged or rotten for restoration, they have to extract it. It includes removing the damaged tooth to prevent infection and pain, followed by conversations about replacement options such as dental implants or bridges, if necessary.
1. Root Canal
Root Canal treatment is a dental procedure for repairing severely compromised or infected teeth. A root canal involves extracting the infected or inflammatory pulp from the tooth, cleaning and disinfecting the interior, and sealing the tooth to prevent further infection. It is required when a patient has a decayed, infected, or wounded tooth but has enough functional tooth structure to support surgery. Root canal therapy consists of removing infected pulp, washing and disinfecting the area, filling and sealing the tooth, administering local anaesthesia, isolating it in a rubber dam, and making an incision in the crown to reach the pulp chamber and root canals.
Root canal therapy consists of removing the affected pulp, cleaning and disinfecting the area, and sealing the tooth to prevent further infection. The endodontist administers local anaesthesia to guarantee the patient's comfort and isolates the tooth with a rubber dam. An incision is performed in the crown to access the pulp chamber and root canals. The canals are filled and sealed with biocompatible substances like gutta-percha. A dental crown is sometimes used to provide structural integrity. Clinical trials and studies have shown that root canal therapy relieves pain associated with dental infections and saves teeth.
2. Endodontic Retreatment
Endodontic Retreatment is recommended for teeth with radiographic evidence of apical periodontitis and clinical symptoms of inflammation. Endodontic retreatment is required when a tooth treated with root canal therapy fails to heal adequately or develops new problems over time. The root canal filling becomes infected due to insufficient cleaning during the first treatment, intricate canal features initially missed, or fresh deterioration exposing the filling to germs. A new fracture or lesion to a tooth compromises the previous root canal treatment's integrity. Persistent symptoms such as pain, swelling, or tenderness in the treated area signal the need for a retreatment.
Endodontic retreatment involves the endodontist reopening the tooth, removing the previous filling materials, thoroughly cleaning and reshaping the canals, and refilling and sealing them to encourage healthy healing and retain the natural tooth. The treatment is intended to maintain good oral health for a long time. The endodontist explains different treatment choices, including retreatment, which entails reopening the tooth to obtain root canal filling material. The endodontist cleans the canals and inspects the inside for additional canals or abnormal morphology. Endodontic surgery is recommended if the canals are small or clogged. A new crown or restoration is implanted after retreatment to safeguard and restore the tooth's functionality.
3. Endodontic Surgery
Endodontic Surgery is performed to preserve a tooth beyond saving with root canal therapy or to correct complications connected with a root canal. Endodontic surgery is required when traditional root canal therapy fails to resolve an underlying tooth condition or when complications emerge that are not treated nonsurgically. An apicoectomy, a surgical procedure, is recommended when the root tip remains inflamed or infected following root canal therapy. It is required when the root structure is exceptionally complicated, making it challenging to thoroughly clean and close the root canals during the first treatment. Endodontic surgery is required to remove calcium deposits from the root canals, repair damaged root surfaces or surrounding bone, and treat chronic cysts or abscesses. Endodontic surgery is necessary if there is persistent pain, oedema, or recurrence of symptoms after prior therapy. Endodontic surgery aims to save the tooth, stop more damage, and improve general oral health by surgically removing the infected tissue and closing the root end.
The procedure begins with the endodontist providing local anaesthesia to numb the area surrounding the afflicted tooth, ensuring the patient's comfort. The endodontist makes a small incision in the gum tissue next to the tooth to reach the root and underlying bone. The endodontist exposes the gum tissue near the tooth to expose the underlying bone and remove any inflammatory or infected tissues. The very end of the root is removed. A little filler is inserted in the root to seal the end of the root canal, and a few stitches or sutures are placed in the gingiva to aid in tissue healing. Bone heals around the root's end.
4. Emergency Dental Surgery
Emergency Dental Surgery includes problems with teeth and supporting tissues, which are often painful. Pain comes from the tooth, the surrounding tissues, or another cause. Symptoms include bacterial, fungal, or viral infections and damaged teeth or dental restorations. Each emergency requires a specific treatment and response. Early treatment for fractures, missing restorations, and tooth tissue loss is recommended. Dental emergencies necessitate professional intervention to maintain teeth for a long time.
Emergency dental surgery is necessary when a patient has severe dental problems that require immediate attention to treat life-threatening disorders, prevent further damage, or relieve pain. Traumatic injuries such as fractured teeth, severe tooth infections or abscesses causing significant pain and swelling, uncontrolled bleeding after dental trauma, and conditions that obstruct breathing or swallowing are reasons for emergency dental surgery. Emergency dental surgery stabilises the patient, treats the immediate problem, and avoids consequences.
The procedure starts with the endodontist examining the tooth to determine what needs to be done. Local anaesthesia relieves discomfort and keeps the patient comfortable during the treatment. Surgical procedures include extraction of a tooth that is not saved, reimplantation of a damaged tooth, draining an abscess, or making an incision to release pressure and remove contaminated tissue, depending on the severity of the emergency. Treating soft tissue injuries and stabilising fractured jawbones is part of the surgery in cases of severe trauma.
The patient receives comprehensive post-operative care instructions to promote healing and avert complications after the urgent problem is resolved. Follow-up sessions are scheduled to monitor the healing process and plan extra treatments to restore the patient's oral health. Emergency dental surgery is essential for delivering immediate relief and preserving oral function in emergency conditions.
5. Tooth Extraction
Tooth Extraction is the dental treatment of removing a tooth from its socket in the jawbone. The dental procedure is performed when a tooth is severely deteriorating, infected, wounded, or threatens the patient's dental health. Addressing various dental issues and preventing infections from spreading or injuring surrounding teeth is critical. It extracts a tooth from its jawbone socket, followed by a comprehensive examination and X-rays. A topical anaesthetic alleviates pain, and the tooth is carefully extracted with specialised equipment. Post-operative care includes instructions on managing edema, avoiding specific foods, and taking prescribed medications. Getting a tooth extracted is crucial for avoiding problems, improving oral health, and preparing patients for future dental procedures. Open communication between patients and dentists is critical for understanding postoperative care and tooth replacement alternatives.
Tooth extraction procedures vary depending on the tooth’s condition. For example, a wisdom tooth extraction is a standard dental procedure that requires a thorough X-ray evaluation to establish the best extraction method. Local anaesthesia is used for painless procedures, but general anaesthesia is necessary for a more complex tooth extraction. An incision in the gum tissue is made to access the tooth, gently extracted with specialised equipment. The incision is sutured closed following the procedure. Wisdom teeth extractions treat and prevent discomfort, infection, and cyst formation. Patients expect pain reduction and fewer dental health concerns.
Do Endodontists use Laser Treatment?
Yes, endodontists use laser treatment. Endodontics now offers modern laser equipment that uses multiple wavelengths and materials to meet diverse demands. Lasers are more precise and less invasive than traditional dental technology, providing more significant results and faster healing times. Endodontic treatments use lasers as therapy coadjuvants, with low-intensity laser therapy (LILT) and high-intensity laser treatment (HILT) used to improve clinical operation success rates. LILT has analgesic, anti-inflammatory, and modulatory effects on irradiated soft tissue, which enhances wound healing and the postoperative experience. High-intensity laser irradiation is used on hard dental tissues to alter structural morphology, remove smear layers, melt and recrystallise dentine, and expose dentinal tubules.
Endodontic laser treatment has many advantages, including better precision, less pain, and faster recovery. Lasers are more successful than traditional cleaning and disinfecting root canals because their light energy can reach bacteria and debris deep into the root systems. Lasers aid in redesigning and sealing the root canals, increasing the overall effectiveness rate of root canal treatment. Laser dentistry is considered less invasive, which helps patients recover faster by reducing their discomfort and swelling. Endodontists use the new method to deliver more efficient and comfortable care in complex or re-treatment cases.
What to Expect after an Endodontic Procedure?
Mild and moderate discomfort and sensitivity are expected after an endodontic procedure. Most patients recover well from endodontic operations and improve after treatment. The treated tooth functions effectively for a prolonged period if it is well cared for and monitored. Discomfort is alleviated with over-the-counter pain medications such as ibuprofen or acetaminophen. Swelling and soreness at the gum line near the treated tooth are common but disappear in a few days. Patients are advised to avoid biting on the treated side of their mouth until the healing process is well started and to eat a soft diet at first to avoid irritation.
Adhering to post-operative care guidelines given by the endodontist is crucial. The instructions involve cleaning the area, using a mouth rinse suggested by the doctor, and scheduling follow-up appointments to track the healing process. A general dentist needs to replace a temporary filling or crown that was set during the operation with a permanent restoration. Patients must contact their endodontist immediately for additional assessment and care if they experience unusual issues, such as excruciating pain, persistent swelling, or infection-related symptoms like fever or pus discharge.
What are the Advantages of Endodontic Treatment?
The advantages of endodontic treatment are listed below.
- Painless: Endodontic treatment is painless. Modern dental techniques and anaesthesia have made root canal therapy pleasant for patients. Local anaesthetic numbs the affected tooth and surrounding tissues, ensuring patient comfort during treatment. Clients with dental anxiety or sensitivity are given anaesthesia, which makes the root canal procedure even less painful for them.
- Economical and Effective: Endodontic treatment is an efficient and cost-effective solution to preserve healthy teeth and gums while saving patients time and money. The hassle associated with more intrusive treatments, such as dental implants or bridges, costs more than traditional root canals.
- Stops Toothaches: Endodontic treatment removes inflammatory or damaged pulp tissue from the tooth, reducing discomfort. Root canals improve oral comfort and provide long-term relief by addressing the underlying cause of toothaches, allowing patients to grin, eat, and speak without pain or sensitivity.
- Preserve the Natural Tooth: Root canal therapy preserves the natural tooth structure, including the roots and surrounding bone, instead of extraction, which removes the entire tooth. It prevents problems like shifting teeth and jawbone degeneration after tooth loss by preserving jawbone integrity and aiding in the proper alignment of surrounding teeth.
- Avoids Gaps Between Teeth: Gaps or spaces left between teeth following tooth extraction affect speech, bite alignment, and attractiveness. Root canal therapy preserves the original tooth structure by removing gaps and ensuring sufficient spacing and alignment within the dental arch. It promotes optimal oral health by providing the bite's harmony and functionality.
- Prevents Spreading of Diseases: Untreated dental infections result in more severe dental issues and even systemic health concerns as they spread to the gums, nearby teeth, and jawbone. Root canal therapy prevents the infection from spreading. It reduces the risk of complications such as oral discomfort or the formation of an abscess by removing infected tissue and sealing the tooth.
- Fantastic Result: A dental crown or filling is utilised to repair the tooth after root canal therapy, resulting in an aesthetically pleasing and natural-looking outcome. Dental crowns are precisely manufactured to match the colour, contour, and shape of the original teeth, increasing attractiveness and blending into the smile. Patients smile and communicate more effectively because the restored tooth functions normally.
What are the Risks of an Endodontic Treatment?
The risks of an endodontic treatment include infection, tooth fractures, discomfort, and sensitivity. Patients must be aware of the risks associated with endodontic therapy, considering it is safe and successful. One of the significant risks is the threat of chronic infection. Bacteria survive or re-enter the treated area despite thoroughly cleaning and sealing the root canals. It results in persistent infection and the need for extra treatment or surgery. Tooth fractures are another concern. Teeth that have received endodontic treatment become more brittle and prone to cracking or fracturing, particularly if not fully repaired with a crown or other protective devices.
Patients feel slight discomfort or sensitivity after the treatment, which is tolerable with over-the-counter pain drugs but concerning for some. There is a minor risk of procedural problems, such as accidental damage to adjacent tissues or nerves, which cause numbness or altered sensation in the affected area. An infection, in rare instances, spreads to other parts of the body and causes more significant health problems if it is left untreated or improperly handled.
Are Procedures Performed by Endodontists Painful?
No, procedures performed by endodontists are not painful. Modern developments in dental methods and anaesthesia help eliminate pain. Endodontic treatments such as root canals or operations are performed under local anaesthesia, providing the patient with comfort and a pain-free experience. The anaesthetic prevents pain from reaching the brain, allowing the endodontist to work on the tooth while causing no discomfort. Patients experience pressure or minor movement, but it is not uncomfortable.
Some mild to moderate soreness and sensitivity following the operation are expected when the anaesthesia wears off, and the tissues start healing. Over-the-counter pain medications such as ibuprofen or acetaminophen are effective for managing post-treatment pain. The endodontist gives patients aftercare instructions to help them feel better and recover faster. Endodontic treatments are frightening, but patients find them comfortable due to advances in dental care. The short discomfort felt following treatment is overshadowed by the relief from pain and infection that such treatments give, leading to improved oral health.
Some discomfort is expected due to the treatment's intrusive nature, the tooth's pre-existing condition, and the healing process. Endodontists take steps to reduce discomfort and promote patient comfort before and after the treatment, and post-operative care instructions are supplied to help with recovery. Pain is caused by the type of underlying tooth problem, the complexity of the procedure, and the body's natural response to surgery. Endodontic intervention is necessary for the tooth's and surrounding tissues' inflammation or infection, which causes excruciating pain before the procedure. Local anaesthesia successfully numbs the area throughout the treatment, but patients continue to feel pressure or vibrations, which is disturbing.
Patients suffer pain or sensitivity after the treatment as the anaesthesia wears off and the treated area heals. The post-procedure soreness is often mild to moderate and is treated with over-the-counter pain medications. Swelling and discomfort are normal and part of the body's natural healing process. Recurring infections or tissue irritation are rare implications that lead to chronic pain and require additional care.





