Dry mouth (xerostomia) is a condition characterised by a lack of adequate saliva in the mouth. A dry mouth leads to significant discomfort, dental problems, and difficulty in daily activities such as speaking and swallowing. Understanding the symptoms, treatment options, and causes of dry mouth is crucial for effective management. Exploring similar conditions and current research provides a comprehensive view of xerostomia and its implications.
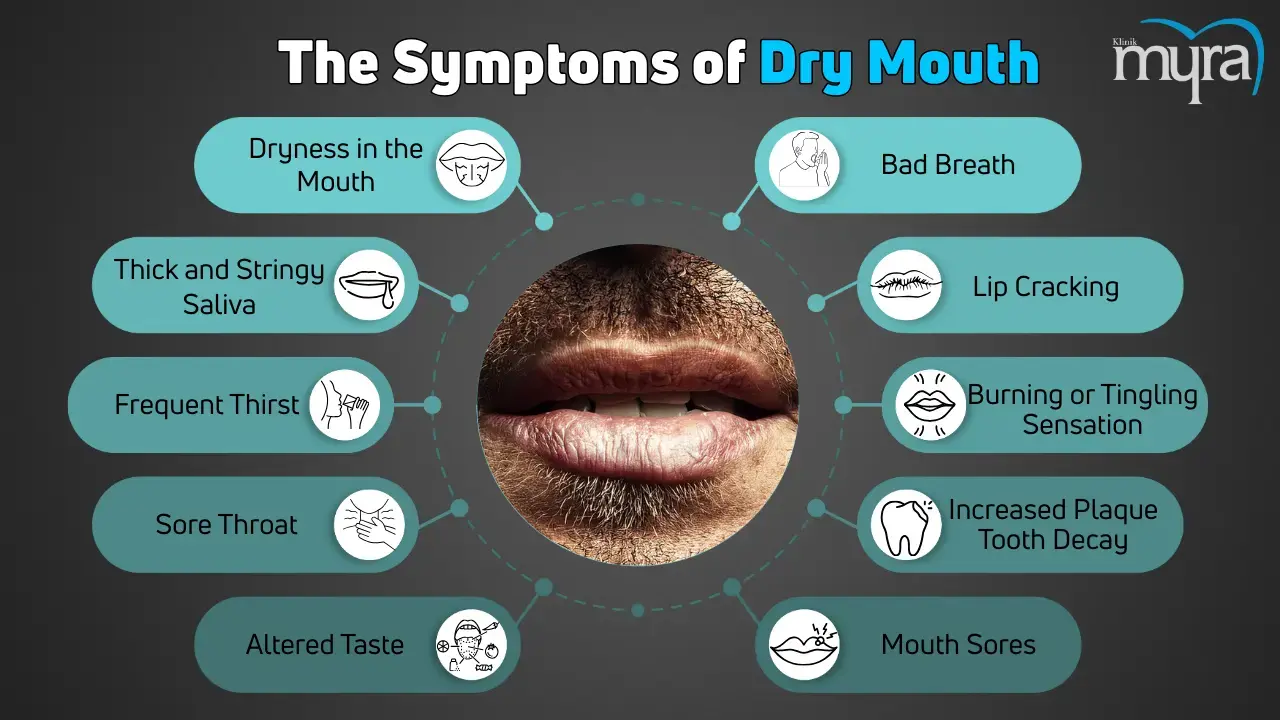
The symptoms of dry mouth are quite noticeable and affect oral health and quality of life. Common symptoms include a persistent feeling of dryness and stickiness in the mouth, thick and stringy saliva, frequent thirst, a dry or grooved tongue, and a sore throat. Patients experience difficulty speaking and swallowing, changes in taste, bad breath, and cracked lips. Dry mouth leads to mouth sores, increased plaque, tooth decay, and gum disease due to the lack of saliva’s protective effects in severe cases.
Treatment for dry mouth focuses on alleviating symptoms and addressing underlying causes. Increasing fluid intake is a simple yet effective way to manage mild cases. Over-the-counter saliva substitutes and mouthwashes designed for dry mouth provide relief. Chewing sugar-free gum or sucking on sugar-free candies stimulates saliva production. Good oral hygiene practices, such as brushing with fluoride toothpaste and using alcohol-free mouthwash, are essential to prevent dental complications. Prescription medications like pilocarpine and cevimeline are recommended to stimulate saliva production.
The causes of dry mouth are varied and include medication side effects, systemic diseases, lifestyle factors, and medical treatments. Medications such as antihistamines, decongestants, painkillers, and antidepressants are common culprits. Systemic diseases like Sjögren's syndrome, diabetes, and HIV/AIDS affect saliva production. Lifestyle factors such as smoking, alcohol consumption, and dehydration contribute to dry mouth. Treatments like radiation therapy for head and neck cancers damage salivary glands, leading to xerostomia.
Conditions similar to dry mouth include a range of oral and systemic disorders that impact moisture levels and comfort in the mouth. Examples include dry scalp, seborrheic dermatitis, psoriasis of the scalp, eczema, and lichen planopilaris. These conditions share similarities with dry mouth regarding dryness and discomfort while affecting different body parts. Managing these conditions involves similar approaches, such as moisturising treatments and addressing underlying causes.
Research into dry mouth continues to advance, focusing on understanding its aetiology, impacts, and treatment options. Notable researchers include Dr. Christopher Fox, who has explored the relationship between xerostomia and systemic diseases, and Dr. Joel Epstein, known for his work on managing dry mouth in cancer patients. Studies aim to develop better saliva substitutes, improve understanding of the condition's pathophysiology, and find new ways to protect oral health. Innovations in treatment, such as advanced saliva stimulants and protective dental technologies, are being investigated to improve patient outcomes.
What are the Types of Dry Mouth?
The types of Dry Mouth are listed below.
- Drug-induced Dry Mouth: Drugs such as antihistamines, decongestants, pain medications, diuretics, and antidepressants cause drug-induced dry mouth. These medications reduce saliva production as a side effect.
- Disease-related Dry Mouth: Disease-related dry mouth is associated with certain medical conditions, such as Sjögren's syndrome, diabetes, HIV or AIDS, Alzheimer's disease, and Parkinson's disease. These conditions directly affect salivary gland function or reduce saliva production.
- Dehydration-induced Dry Mouth: Dehydration-induced dry mouth results from insufficient fluid intake, excessive sweating, fever, vomiting, diarrhoea, or blood loss. Dehydration decreases saliva production.
- Radiation-induced Dry Mouth: Radiation-induced dry mouth occurs in patients undergoing radiation therapy for head and neck cancers. Radiation damages salivary glands, leading to reduced saliva production.
- Nerve Damage-related Dry Mouth: Nerve damage-related dry mouth is caused by injury or surgery that results in nerve damage to the head and neck area. The damage impairs the nerves that control salivary glands, reducing saliva production.
- Lifestyle-induced Dry Mouth: Lifestyle-induced dry mouth is linked to lifestyle factors such as smoking, alcohol consumption, and use of recreational drugs. These habits reduce saliva production or affect the salivary glands.
- Ageing-related Dry Mouth: Aging-related dry mouth is common in older adults, as ageing naturally reduces saliva production. Older adults take medications that cause dry mouth.
- Breathing-related Dry Mouth: Breathing-related dry mouth results from chronic mouth breathing due to nasal congestion or sleep apnea. Breathing through the mouth dries out the oral tissues.

What are the Symptoms of Dry Mouth?
The Symptoms of Dry Mouth are listed below.
- Dryness and Sticky Feeling in the Mouth: Dryness and sticky feeling in the mouth are persistent feelings of dryness, and stickiness in the mouth is one of the most noticeable symptoms.
- Thick and Stringy Saliva: Saliva becomes denser and more stringy than usual.
- Frequent Thirst: An increased need to drink water or other fluids frequently.
- Sore Throat: A dry mouth leads to a sore throat and hoarseness.
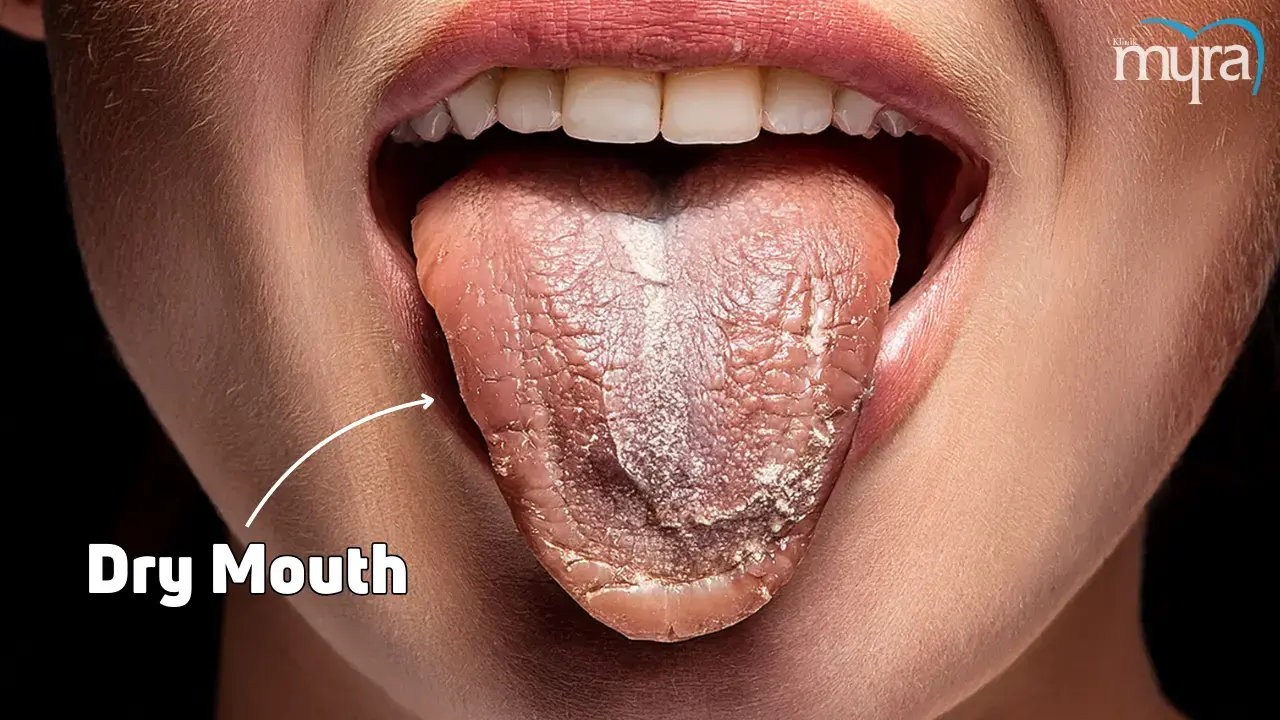
- Dry or Grooved Tongue: The tongue appears dry and grooved.
- Difficulty in Speaking and Swallowing: A lack of saliva makes it hard to speak clearly and swallow food or liquids.
- Altered Taste: Changes in taste or a metallic taste in the mouth.
- Bad Breath: Persistent bad breath (halitosis) results from dry mouth.
- Dryness in the Nasal Passages: A dry mouth leads to a dry feeling in the nasal passages.
- Lip Cracking: The lips in the corners crack and become sore.
- Burning or Tingling Sensation: A burning or tingling sensation in the mouth on the tongue.
- Increased Plaque, Tooth Decay, and Gum Disease: Reduced saliva leads to a higher risk of dental problems, as saliva helps to wash away food particles and neutralise acids produced by bacteria in the mouth.
- Mouth Sores: Development of mouth sores or mouth ulcers in the mouth.
- Difficulty Wearing Dentures: A dry mouth makes it uncomfortable or difficult to wear dentures.
What are the Causes of Dry Mouth?
The Causes of Dry Mouth are listed below.
- Medications: Prescription and over-the-counter medications cause dry mouth as a side effect. Medication includes antihistamines, decongestants, pain medications, diuretics, muscle relaxants, and antidepressants.
- Medical Conditions: Certain medical conditions lead to dry mouth. Medical conditions include Sjögren's Syndrome, diabetes, HIV/AIDS, stroke, Alzheimer’s, and Parkinson’s diseases. Sjögren's Syndrome is an autoimmune disorder that targets the salivary glands. Diabetes is a high blood sugar level that reduces saliva production. HIV/AIDS is a virus, and some medications used to treat it cause dry mouth. Alzheimer's Disease affects the perception of dryness and prompt fluid intake. Parkinson's Disease leads to reduced saliva production. Stroke causes dry mouth due to neurological effects.
- Radiation Therapy: Radiation treatment for head and neck cancers damages the salivary glands, reducing saliva production.
- Chemotherapy: Chemotherapy drugs change the nature of saliva and how much is produced.
- Nerve Damage: Injury or surgery that results in nerve damage to the head and neck area impairs the nerves that control the salivary glands.
- Dehydration: A lack of sufficient fluid intake, excessive sweating, fever, vomiting, diarrhoea, or blood loss lead to dehydration and dry mouth.
- Lifestyle Factors: Lifestyle factors such as smoking, alcohol consumption, and recreational drug use. Tobacco use affects saliva production and causes dry mouth. Alcohol has a drying effect on the mouth. Certain drugs, such as methamphetamine and marijuana, reduce saliva production.
- Breathing Through the Mouth: Chronic mouth breathing due to nasal congestion or sleep apnea leads to dry mouth.
- Ageing: Aging reduces saliva production, and older adults take medications that cause dry mouth.
- Hormonal Changes: Hormonal changes, particularly in women related to menopause, affect saliva production and lead to dry mouth.
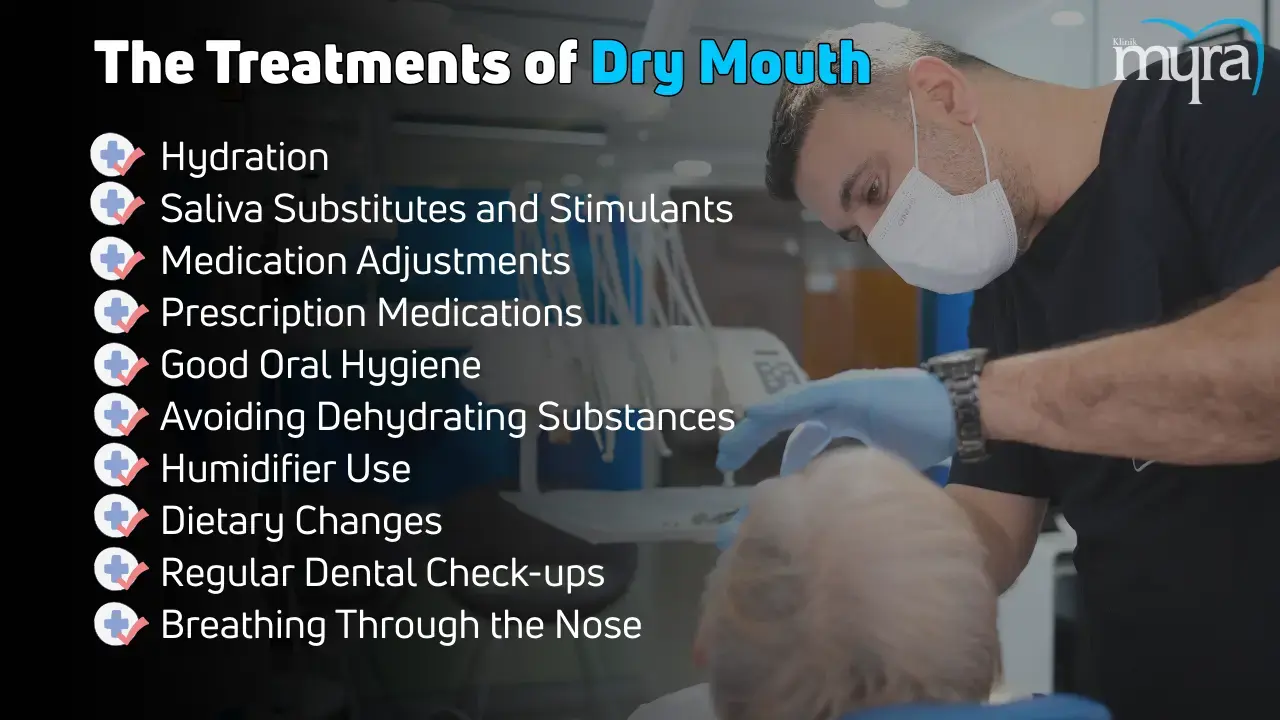
What are the Treatments of Dry Mouth?
The Treatments of Dry Mouth are listed below.
- Hydration: Increasing fluid intake helps alleviate dry mouth symptoms. Drinking water regularly throughout the day is essential.
- Saliva Substitutes and Stimulants: Over-the-counter saliva substitutes and mouthwashes designed for dry mouth provide relief. Chewing sugar-free gum or sucking on sugar-free candies stimulates saliva production.
- Medication Adjustments: A healthcare provider adjusts the dosage or switches to a different medication if medications are causing dry mouth.
- Prescription Medications: Medications like pilocarpine (Salagen) and cevimeline (Evoxac) stimulate saliva production and are prescribed for severe dry mouth.
- Good Oral Hygiene: Maintaining good oral hygiene helps prevent complications. Good oral hygiene includes brushing with fluoride toothpaste, flossing regularly, and using an alcohol-free mouthwash.
- Avoiding Dehydrating Substances: Reducing or eliminating caffeine, alcohol, and tobacco helps manage dry mouth symptoms.
- Humidifier Use: A humidifier at night adds moisture to the air and helps keep the mouth hydrated.
- Dietary Changes: Avoid salty, spicy, and acidic foods to prevent irritation and dryness. Opt for soft, moist foods and use sauces or gravies to make food easier to swallow.
- Regular Dental Check-ups: Regular visits to the dentist are essential for monitoring oral health and managing any dental issues that arise from dry mouth.
- Breathing Through the Nose: Addressing nasal congestion or sleep apnea helps if mouth breathing contributes to dry mouth. Breathing exercises and treatments for nasal congestion are beneficial.
- Specialised Mouthwash: Mouthwashes formulated for dry mouth help keep the mouth moist and protect against cavities.
Can Dry Mouth Be Treated At Home?
Yes, dry mouth can be treated at home using various methods to alleviate symptoms and improve saliva production. Increasing fluid intake is one of the simplest and most effective ways to combat dry mouth. Drinking plenty of water throughout the day helps keep the mouth hydrated and maintains moisture levels. Chewing sugar-free gum or sucking on sugar-free candies stimulate saliva production, providing relief from dryness.
Over-the-counter saliva substitutes, such as mouth sprays and gels, are beneficial. These products mimic natural saliva and help keep the mouth moist. Maintaining good oral hygiene is crucial; brushing with fluoride toothpaste, flossing regularly, and using an alcohol-free mouthwash prevent dental issues that arise from dry mouth.
Another important step is to avoid dehydrating substances like caffeine, alcohol, and tobacco. These substances exacerbate dry mouth symptoms, so reducing or eliminating their use provides significant relief. Using a humidifier at night adds moisture to the air, helping to keep the mouth hydrated during sleep.
Adjusting the diet to avoid salty, spicy, and acidic foods prevents further irritation and dryness. Opting for soft, moist foods and using sauces or gravies make eating more comfortable. Practising nasal breathing instead of mouth breathing helps prevent dryness. Addressing any nasal congestion issues is important to ensure breathing through the nose is possible.
These home treatments effectively manage mild to moderate dry mouth symptoms. Consult a healthcare provider if symptoms persist or are severe, as they indicate an underlying medical condition requiring professional treatment.
What are the Researches about Dry Mouth?
The research about dry mouth (xerostomia) encompasses various aspects, including its causes, effects, treatment options, and impacts on quality of life. Studies investigate the underlying causes of dry mouth, such as the role of medications, systemic diseases like Sjögren's syndrome and diabetes, and cancer treatments like radiation therapy. Research explores the pathophysiological mechanisms leading to reduced saliva production, including the effects of autoimmune responses and nerve damage.
Research focuses on the consequences of dry mouth on oral health, including increased risk of dental caries, periodontal disease, oral infections, and difficulties with speaking, chewing, and swallowing. Studies examine the correlation between dry mouth and the development of conditions like oral candidiasis and mucositis.
The research “Salivary Gland Dysfunction in Patients with Sjögren’s Syndrome: A Comprehensive Review” examines the pathophysiology, clinical manifestations, and diagnostic methods for salivary gland dysfunction in patients with Sjögren’s syndrome. The study discusses the impact of reduced saliva production on oral health, quality of life, and complications. Researchers explore treatment options, including artificial saliva substitutes and immunomodulatory therapies.
Investigations assess the impact of dry mouth on patients' quality of life, including psychological effects, social interactions, and daily activities. Surveys and clinical studies measure patient-reported outcomes and satisfaction with various treatments.
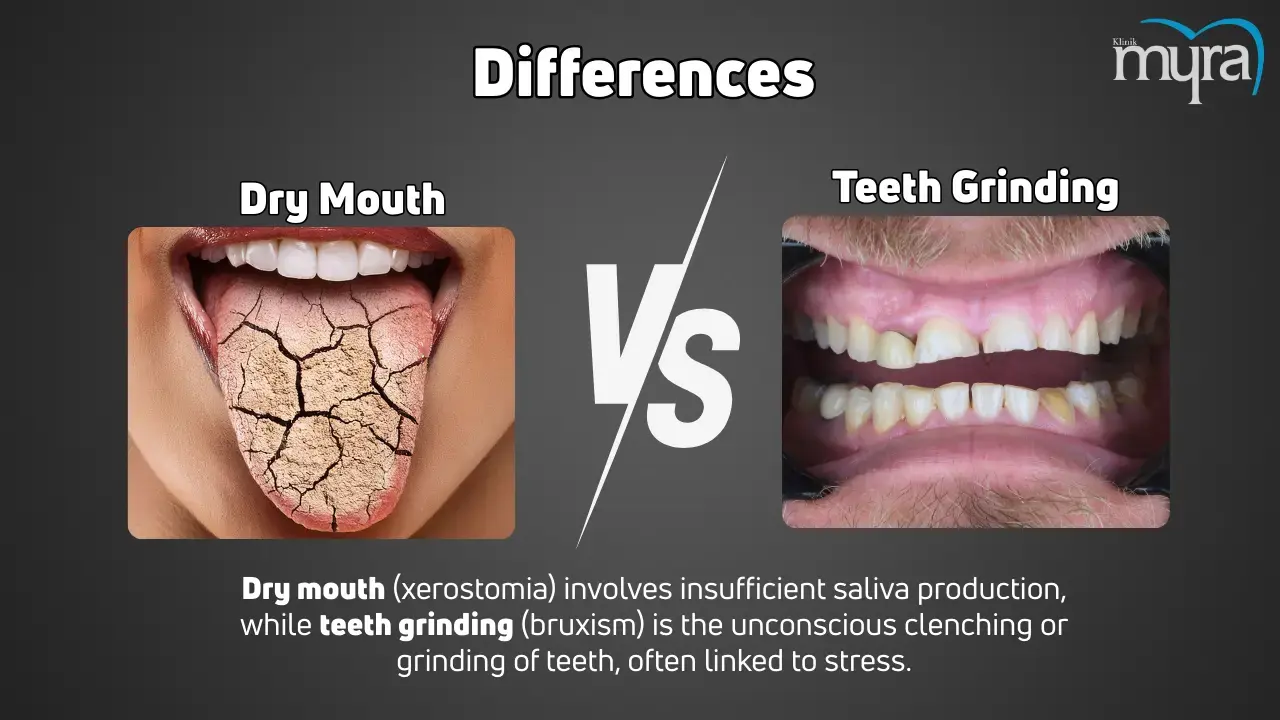
What are the Differences between Dry Mouth and Teeth Grinding?
The difference between dry mouth and teeth grinding lies primarily in their underlying causes and treatment methods. Dry mouth (xerostomia) and teeth grinding (bruxism) are distinct dental issues with unique causes, symptoms, and treatments. A dry mouth involves insufficient saliva production, leading to a persistent feeling of dryness and discomfort. Teeth grinding is characterised by unconsciously clenching or grinding teeth during sleep. These conditions differ significantly in their aetiology and management but share similarities in their impact on oral health.
The causes of dry mouth and teeth grinding are quite different. Dry mouth is a side effect of medications, such as antihistamines, decongestants, painkillers, and antidepressants. It results from medical conditions like Sjögren's syndrome, diabetes, HIV/AIDS, and radiation therapy for head and neck cancers. Lifestyle factors such as smoking, alcohol consumption, and dehydration contribute to dry mouth. Teeth grinding is caused by stress and anxiety, sleep disorders like sleep apnea, an abnormal bite, or missing and crooked teeth. It is a side effect of certain medications, such as antidepressants.
Treatments for dry mouth focus on increasing saliva production and maintaining oral moisture. It involves sipping water frequently, using saliva substitutes, chewing sugar-free gum, and using alcohol-free mouthwashes. Medications such as pilocarpine and cevimeline are prescribed to stimulate saliva production in more severe cases. Good oral hygiene practices are crucial to prevent complications like tooth decay and gum disease. Treatments for teeth grinding aim to reduce the grinding and protect the teeth from damage. Stress management techniques, including relaxation exercises and therapy, help address the underlying anxiety or stress. Dental appliances like mouthguards or splints are commonly used to protect the teeth during sleep. Medications such as muscle relaxants or Botox injections are recommended to reduce muscle activity.
Dry mouth and teeth grinding share similarities in their impact on oral health. Dry mouth and teeth grinding lead to significant dental problems if not appropriately managed. A dry mouth increases the risk of tooth decay, gum disease, and oral infections due to the lack of saliva's protective effects. Teeth grinding causes tooth wear, fractures, sensitivity, jaw pain, and headaches. Dry mouth and teeth grinding highlight the importance of addressing dental issues promptly to prevent long-term damage and maintain oral health.
Dry mouth and teeth grinding which means bruxism are distinct conditions with different causes and treatments. Dry mouth is related to medication use, medical conditions, and lifestyle factors, while teeth grinding is linked to stress, sleep disorders, and dental issues. Treatment approaches vary accordingly, focusing on increasing saliva production, managing stress, and protecting teeth. However, both conditions underscore the critical role of maintaining good oral hygiene and seeking professional dental care to prevent complications.